-
80-3465 Platinum Drive,
Mississauga, ON, L5M 2S1
-
Mon – Fri: 9:00 AM to 6:00 PM
Sat – Sun: 10:00 AM to 6:00 PM
 Average Risk
Average RiskThe Ontario Breast Screening Program recommends that most eligible women, trans and non binary people ages 50 to 74 get screened with mammography every 2 years.
People ages 50 to 74 are eligible for screening through the Ontario Breast Screening Program if they:
• have no new breast cancer symptoms
• have no personal history of breast cancer
• have no current breast implants
• have not had a mastectomy
• have not had a screening mammogram within the last 11 months
The Ontario Breast Screening Program recommends that people ages 30 to 69 who meet the High-Risk Ontario Breast Screening Program eligibility criteria get screened every year with both mammography and breast magnetic resonance imaging (MRI) (or screening breast ultrasound if MRI is not medically appropriate).
 • Getting screened regularly with mammography is important because it can find cancer early when it is less likely to have spread to other parts of the body. Treatment may also have a better chance of working when breast cancer is found early.
• Getting screened regularly with mammography is important because it can find cancer early when it is less likely to have spread to other parts of the body. Treatment may also have a better chance of working when breast cancer is found early.
• When breast cancer is found early, almost all people will survive for 5 years. However, if breast cancer is found later, only 2 out of 10 people will survive for 5 years.
Normal screening result
• The Ontario Breast Screening Program directly notifies participants (with or without a primary care provider) of their normal results by mail. The letter will also tell participants when to get screened again.
• The screening site also sends normal screening results to a screening participant’s primary care provider.
Abnormal screening result
• Most people with abnormal mammograms do not have breast cancer. More tests are needed after an abnormal mammogram to determine whether a person has cancer.
• Additional testing may include more mammography, breast ultrasound, breast magnetic resonance imaging and/or biopsies.
• After a participant has an abnormal screening result, their screening site will notify their primary care provider and may help to schedule a timely follow-up appointment.
 A participant with an abnormal mammogram who does not have a primary care provider will be assigned to a doctor by their screening site to follow them to diagnosis. If the participant does have breast cancer, they will be referred to a specialist for further care and management.
A participant with an abnormal mammogram who does not have a primary care provider will be assigned to a doctor by their screening site to follow them to diagnosis. If the participant does have breast cancer, they will be referred to a specialist for further care and management.
A Pap test is a quick and simple screening tool that detects atypical and abnormal cell changes in the cervix that may lead to cancer. Cells can become abnormal, and they die and renew, or when a woman has contracted human papillomavirus (HPV) infection.
It does not test for other cancers in the reproductive organs or for sexually transmitted infections (STI); however chlamydia and gonorrhea screening can be performed at the same time as your pap test.
The Ontario Cervical Screening Program recommends that women who have been sexually active or are currently sexually active receive a pap test every 3 years between the ages of 25-70. Pap tests can stop at the age of 70 if you have had 3 or more normal tests in the last 10 years.
Try to make your appointment on a day you are not menstruating. Do not have sex or use tampons, vaginal creams or medicine for 48 hours before the test. If these measures cannot be taken, still attend your appointment.
HPV is a common cause of cervical cell changes. HPV is a family of viruses that most people contract through sexual contact at some point in their lifetime. It is typically an asymptomatic virus and goes away naturally within 1 – 2 years. However, in some cases, the virus survives in the body and slowly leads to cancer through causing abnormal cervical cell changes. The HPV vaccine can protect against HPV infection.
Cancer Care Ontario offers an online risk assessment tool to help you educate yourself about certain family and personal factors that may be increasing or decreasing your risk for cervical cancer. At the conclusion of the assessment, you will receive personalized tips on how to lower your risk and become proactive in regard to your health and cancer prevention.
 Colorectal cancer is a disease in which cells in the colon or rectum grow out of control. Sometimes it is called colon cancer, for short. The colon is the large intestine or large bowel. The rectum is the passageway that connects the colon to the anus.
Colorectal cancer is a disease in which cells in the colon or rectum grow out of control. Sometimes it is called colon cancer, for short. The colon is the large intestine or large bowel. The rectum is the passageway that connects the colon to the anus.
Your risk of getting colorectal cancer increases as you get older. Other risk factors include having—
• Inflammatory bowel disease such as Crohn’s disease or ulcerative colitis.
• A personal or family history of colorectal cancer or colorectal polyps.
• A genetic syndrome such as familial adenomatous polyposis (FAP)external icon or hereditary non-polyposis colorectal cancer (Lynch syndrome).
• The guaiac-based fecal occult blood test (gFOBT) uses the chemical guaiac to detect blood in the stool.
• The fecal immunochemical test (FIT) uses antibodies to detect blood in the stool. It is also done once a year in the same way as a gFOBT.
• The FIT-DNA test (also referred to as the stool DNA test) combines the FIT with a test that detects altered DNA in the stool. For this test, you collect an entire bowel movement and send it to a lab, where it is checked for altered DNA and for the presence of blood. It is done once every three years.
For this test, the doctor puts a short, thin, flexible, lighted tube into your rectum. The doctor checks for polyps or cancer inside the rectum and lower third of the colon. How often: Every 5 years, or every 10 years with a FIT every year.
This is similar to flexible sigmoidoscopy, except the doctor uses a longer, thin, flexible, lighted tube to check for polyps or cancer inside the rectum and the entire colon. During the test, the doctor can find and remove most polyps and some cancers. Colonoscopy also is used as a follow-up test if anything unusual is found during one of the other screening tests. How often: Every 10 years (for people who do not have an increased risk of colorectal cancer).
Computed tomography (CT) colonography, also called a virtual colonoscopy, uses X-rays and computers to produce images of the entire colon, which are displayed on a computer screen for the doctor to analyze. How often: Every 5 years.
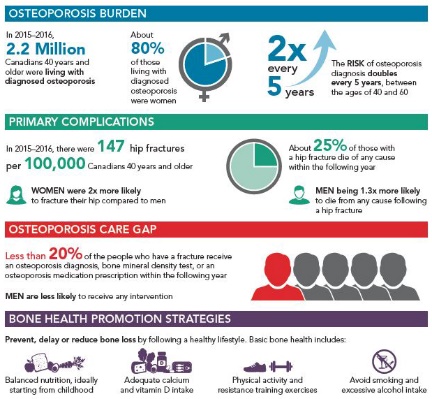 Osteoporosis, a metabolic bone disease characterized by low bone density and an increased risk of fracture, is a major public health concern in Canada and worldwide. It is more common among older people and among women. Despite interventions that have been shown to substantially reduce the risk of osteoporotic fractures, most individuals at high risk of fracture do not undergo appropriate screening or treatment.
Osteoporosis, a metabolic bone disease characterized by low bone density and an increased risk of fracture, is a major public health concern in Canada and worldwide. It is more common among older people and among women. Despite interventions that have been shown to substantially reduce the risk of osteoporotic fractures, most individuals at high risk of fracture do not undergo appropriate screening or treatment.
Osteoporosis occurs when bone tissue loss is faster than normal, causing it to become weak and fracture easily. Often people are not aware they have osteoporosis until a fracture occurs. Common fracture sites include forearm, hip, spine, humerus and pelvis. Hip fractures are among the most serious
As per Osteoporosis Canada (2010), men and women over 65 years should undergo BMD assessment in 1- 3 years with reassessments depending on the risk factors. DEXA of the hip and lumbar spine is the preferred assessment method.
There are different imaging approaches for osteoporosis screening. Dual energy X-ray absorptiometry (DXA or DEXA) is the most common.
A DEXA scan is a noninvasive test that involves passing an X-ray scanner over your body, usually as you are lying down. The X-rays are low dose, which means they have very low radiation levels. DEXA uses two X-ray beams to target both soft tissue and bone, creating a fuller picture of bone health. The whole process takes a few minutes.
DEXA is often directed at the hips and spine, areas prone to fractures. You may be asked to change positions during the scan for better images.
Because the test is noninvasive and involves a very low radiation dose, most people can safely get a DEXA scan. However, notify the technician or doctor if you are pregnant or have hardware or other medical implant devices in the areas to be scanned.
An online tool called FRAX can also be used to evaluate your 10-year possibility of osteoporosis-related bone fractures. FRAX is an algorithm that identifies an individual’s risk factors through a 12-point questionnaire, and responds with a score. FRAX cannot diagnose osteoporosis, but can help you see if further screening or lifestyle changes are advisable.
Basic bone health includes following a bone-healthy diet:
• Balanced nutritional diet
• Adequate calcium and vitamin D intake
• Engaging in regular physical activity and resistance training exercises
• Avoiding smoking and excessive alcohol consumption.
Bone health is important at every age but especially during childhood and adolescence when bones are still growing. As most people reach their maximum bone size and strength (known as peak bone mass) by age 30, bone-healthy behaviours are important from an early age in order to optimize bone health and reduce the risk of developing osteoporosis later in life.
FRAX: https://www.sheffield.ac.uk/FRAX/